
Psoriasis is a pathology in which the human immune system mistakenly attacks healthy skin cells. As a result, scaly plaques appear on its surface, which can be very itchy and even painful. Sometimes the disease is accompanied by inflammation of the joints and eyes.
What is psoriasis?
Psoriasis is a chronic autoimmune disease that causes red, scaly patches to appear on the surface of the skin. These are often called plaques.
Psoriasis cannot be contracted - it is an autoimmune disease, not an infectious disease.
Psoriasis is manifested by inflammation of the skin, as well as abnormally rapid growth and sloughing of cells (keratinocytes) that make up the horny layer - the epidermis. Usually, it is completely renewed in a month, but in people with psoriasis, this process is accelerated many times and takes an average of 3-4 days.

In addition to skin damage, the disease causes joint inflammation (in about 30% of cases). A little less often - in 10% of cases - psoriasis leads to inflammation of the uvea (uveitis).
Prevalence of psoriasis
Psoriasis most often affects people aged 15-35, but in general the disease can appear at any age. The first peak of the appearance of pathology occurs at 15-20 years, the second at 55-60 years.
On average, psoriasis affects approximately 1-2% of people worldwide. In our country, according to the clinical recommendations of the Ministry of Health, in 2021 the prevalence of the disease is 243. 7 cases per 100, 000 population.
Types of psoriasis
Like many chronic diseases, psoriasis differs in stages, severity and form of manifestation.
By stage
Psoriasis has three stages: progressive, stationary and regression (remission) stage.
INprogressive stagered spots appear on the skin. Merging, they form large scaly plaques with a distinct red contour around the edges - it is called erythematous erythema Redness of the skin caused by dilation of capillaries and blood flow. corolla, or corolla. New plaques are very itchy and can hurt.
Traumatized areas of the skin are particularly susceptible to the appearance of new spots: a psoriatic plaque can quickly develop in a place of friction (for example, on clothes), as well as in the area of a scratch or scratch. Doctors call this phenomenon Koebner's phenomenon.
This phenomenon, also known as the "isomorphic reaction", was discovered by the German dermatologist Heinrich Köbner in 1872. The doctor noticed that in some patients with psoriasis, new plaques appeared on the skin at the places of trauma, for example after scratches, injections or bruises.
Stationary stage- stabilization phase. Plaques stop growing, but continue to bother and peel. New rashes and spots usually do not appear.
Regression stageoccurs when psoriasis symptoms begin to disappear. Whitening disappears, plaques lighten and level. Symptoms decrease in this phase.
By weight
To assess the severity of psoriasis, doctors use the PASI system (Psoriasis Area and Severity Index) - an index for assessing the severity and prevalence of psoriasis. It requires a professional analysis of parameters such as severity of erythema, infiltration, peeling and calculation of the skin area affected by rashes.
Depending on the results of the examination, doctors distinguish mild, moderate and severe degrees of the disease.
According to the form
According to the clinical picture of the manifestations, several main forms of psoriasis are distinguished: vulgar, inverse, seborrheic, exudative, guttate, pustular, psoriasis of the palms and soles and psoriatic erythroderma.
Vulgar (ordinary) psoriasis- one of the most common forms, which accounts for about 90% of all cases of the disease. First, red spots appear on the skin, which after a few days transform into raised, scaly plaques. As the plaques develop, they coalesce into large, itchy, scaly lesions. Then the condition enters the stage of stabilization and regression: the manifestations of the disease temporarily subside and the person's well-being improves.
The most common places where psoriasis vulgaris appears are the extensor (outer) skin of the elbows and knees. Lesions also appear on the body and scalp.

Psoriasis vulgaris on the outer part of the elbow
Inverse ("reverse") psoriasisproceeds the same way as usual. The only difference is in the location of the lesions: they appear not on the extensor (outer) part of the knees and elbows, but on the flexor (inner) part - that is, under the knee, under the armpits and in the elbow area, as well as in the neck area, eyelids, navel, inguinal folds. The skin in these places is more delicate, moist and often rubs against clothes. Because of this, it may itch more than in the usual form of the disease, but the peeling in these places is less pronounced.
Seborrheic psoriasisproceeds in the same way as normal, but its foci are located in places with a large number of glands that secrete sebum. This is the scalp, the folds behind the ears, the cheeks and the nasolabial region of the face, the forehead, the chest and the back (mainly the upper part).

Seborrheic psoriasis on the scalp
Exudative psoriasis- a type of disease in which, in addition to peeling, exudate also appears in the lesion. It is a fluid containing protein, some blood cells, and other substances. Exudate can be released from capillaries during inflammation.
The crust on the surface of the plaques in the exudative form of the disease is usually dense, gray-yellow and sometimes slightly moist. This type of psoriasis most often occurs in people with endocrine diseases: thyroid gland pathologies, type 2 diabetes or obesity.
Guttate psoriasisIt does not appear as plaques on the skin, but as multiple papules - swollen spots of bright red color with peeling in the center. The size of the papules can vary from approximately 1 to 10 mm. They mainly cover the torso, arms and legs.
Guttate psoriasis usually occurs in children after streptococcal infections (eg, tonsillitis). It is treated a little better than other types of psoriasis, but in some cases it can turn into a common (vulgar) form.
Pustular psoriasischaracterized by the appearance of multiple pustules on a red erythematous background. Pustules are formations that look a lot like pimples. Such psoriasis can be a consequence of infectious diseases, stress, hormonal imbalance, incorrect use of medicines or inadequate use of ointments. Initially, numerous pustules appear on the red spots. They then merge into one large pus spot (or "pus lake").
The generalized form of pustular psoriasis is difficult to tolerate: with episodes of fever, weakness, as well as severe pain and burning of the skin. Along with this, changes in the nails and joint pain can be observed.
Psoriasis of the palms and soles- typical psoriatic rashes appear in the area of the palms and soles, less often they appear in the form of localized pustular psoriasis. It can affect and deform the nails – they become thicker, dull and uneven.

Psoriasis of the palm
Erythrodermic psoriasisThis is quite rare and is considered an extremely severe form of the disease. There is redness on about 90% of the body, severe itching and pain appear, the skin swells and peels. The temperature often rises and the lymph nodes become inflamed.
Usually, this type of psoriasis is the result of an exacerbation of another form of the disease due to incorrect treatment or adverse environmental factors (for example, sunburn in advanced psoriasis vulgaris, inadequate use of irritating external agents or intravenous administration of glucocorticosteroids).
Symptoms of psoriasis
The manifestations of psoriasis vary depending on the type of disease and its severity.
Common symptoms and signs of psoriasis:
- red, raised, scaly patches on the skin;
- itching in the area of inflammation and peeling;
- changes in the nails: dot prints, thickening and disintegration of the plate, its separation;
- joint pain (sometimes).
For an accurate diagnosis, it is necessary to contact a specialist - a dermatologist.
The mechanism of development of psoriasis
Psoriasis is an autoimmune disease.
All autoimmune pathologies are associated with an error in the functioning of the immune system. Normally, it "scans" the body around the clock and looks for pathogenic cells through foreign protein molecules that distinguish them from the "normal" cells inherent in the body.
As soon as foreign protein molecules are detected, the immune system activates special immune cells - T-lymphocytes, which must destroy the enemy.
But for some people, the friend-foe recognition system can break down. As a result, the immune system begins to attack healthy cells of individual organs or tissues, provokes inflammation in their places and in every way damages the body that it is supposed to protect.
Here's what happens in psoriasis: the immune system attacks the skin. It activates T-lymphocytes and "fixes" them on skin cells. Reaching the target, T-lymphocytes release substances that cause inflammation - cytokines. They provoke the first symptoms: redness, swelling, itching and pain.
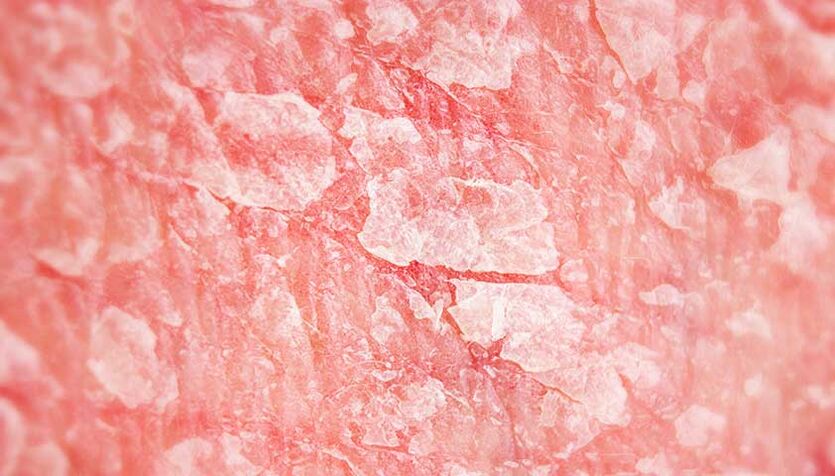
In psoriasis, skin cells divide several times faster, which leads to flakes and peeling.
Under the influence of cytokines, an inflammatory process develops and skin cells begin to actively divide - this is how active peeling occurs and a raised plaque is formed.
Since the cell renewal process is accelerated almost tenfold, the main cells of the epidermis (keratinocytes) do not have time to form properly. And therefore they cannot perform their barrier function.
As a result, the stratum corneum becomes permeable and ceases to protect the deeper layers of the skin from the environment and moisture loss. All this leads to even more inflammation.
Until the immune system calms down, the disease will progress and the symptoms will intensify.
Causes of psoriasis
The exact causes of the development of psoriasis are still not fully understood. However, many studies agree that the development of psoriasis is related to both genetics and lifestyle, comorbidities, and adverse environmental factors.
Genetics
The disease is often inherited from parents to children. Psoriasis is mainly associated with the HLA-C gene. It codes for a protein that allows the immune system to recognize its own (harmless) cells.
In patients with psoriasis, doctors find a special genetic marker in the HLA-C gene more often than in other people - HLA-Cw6. However, its presence only indicates a predisposition to the disease. Not all people with the HLA-Cw6 marker necessarily have psoriasis, and not all patients diagnosed with the disease have this genetic change.
lifestyle
It is believed that permanent damage to the skin, frequent friction, sunburn and hypothermia can be key factors in the development of the disease. Especially if there is a hereditary predisposition in the form of the genetic marker HLA-Cw6 or close relatives suffering from psoriasis.
Other risk factors include constant stress, alcohol abuse and smoking - all of which have a detrimental effect on metabolism, the functioning of internal organs and the immune system.
Concomitant pathologies
Some types of psoriasis, such as guttate psoriasis, can occur after a streptococcal infection.
Also, the risk of developing pathology increases in people with autoimmune diseases. These include, for example, type 1 diabetes, Crohn's disease, systemic lupus erythematosus and rheumatoid arthritis.
In such diseases, the general mechanism of the immune system is disturbed: it perceives some of its own cells as something foreign, reacts with inflammation and destroys them. Accordingly, the risk of her mistakenly adding other cells to the "blacklist" increases.
Complications of psoriasis
Psoriasis is caused by a malfunctioning immune system and chronic systemic inflammation. It develops due to constant aggression of immune cells to healthy tissues.
Autoimmune processes are distinguished by the fact that they can spread: the immune system is able to include other healthy cells in the list of "enemies" at any time.
For example, on the background of psoriasis, Crohn's disease or ulcerative colitis can develop if the immune system mistakenly attacks the tissues of the gastrointestinal tract.
In addition to autoimmune diseases, people with psoriasis are prone to various endocrine pathologies (metabolic syndrome, obesity, type 2 diabetes), cardiovascular diseases (hypertension, heart attack) and other dysfunctions of internal organs. All of this is related to a chronic inflammatory process that affects hormone levels and interferes with normal metabolism.
A separate complication is psoriatic arthritis. It occurs in approximately 30% of people with psoriasis.
In psoriatic arthritis, the immune system attacks the connective tissue, most commonly affecting the joints of the lower extremities. Inflammation of the joint structures develops, the skin in the affected area may redden, there is swelling, and pain and/or stiffness when trying to bend or straighten the joint.
In 10% of people with psoriasis, the pathology spreads to the eyes and develops uveitis. The choroid of the eye becomes inflamed, leading to reduced vision and discomfort.
In addition to the physiological complications, psoriasis can affect a person's mental health. Changes in appearance, poor skin condition and unbearable itching can cause self-doubt and lead to a depressive disorder.
Diagnosis of psoriasis
A dermatologist diagnoses skin diseases, including psoriasis.
At the appointment, the doctor will ask about the symptoms and how long ago they started. Then he will question his closest relatives: parents, brothers and sisters about skin diseases. Family history allows the specialist to immediately assume diseases that can be inherited - psoriasis is one of them.
The doctor will also ask about situations that provoke the appearance of new rashes and worsening of symptoms. For example, new psoriatic lesions may appear after taking a hot bath or prolonged sun exposure. In some patients, plaques appear at the injection sites, scratches or after rubbing the skin on clothes - this is how the Koebner phenomenon, characteristic of psoriasis, manifests itself.
An important point in establishing the diagnosis is the examination of the rash. If the picture of the disease is insufficient, the specialist can monitor the rash over time and prescribe a histological examination of the skin (biopsy).
If the doctor is not sure that the plaques on the skin are psoriasis, he will prescribe a biopsy and a histological examination of the skin.
Histological examination of skin and subcutaneous neoplasms
The examination allows us to identify malignant changes in the tissues of skin tumors (moles, papillomas, warts, age spots). Material obtained by biopsy or during surgery is used for analysis.
In some cases, the specialist may check the psoriasis triad, the main diagnostic signs of psoriasis.
First, the dermatologist will take a glass slide or scalpel and begin to carefully scrape the surface of the plaque. The slight flaking of whitish scales from its surface or the phenomenon of stearic stain is the first sign of the triad.
After all the scabs have peeled off, the surface of the plaque becomes smooth, shiny and slightly moist. This is the second sign of the triad - a terminal film.
If the doctor continues to scratch the area, a point of bleeding will appear on its surface, which is called Auspitz syndrome or blood dew, the third sign of the psoriatic triad.
After an examination and history, the doctor will prescribe laboratory tests. It is usually recommended to do a clinical blood test - it reflects the general state of health. The patient is also referred for blood biochemistry. It allows you to evaluate the functioning of internal organs and metabolism - with a long course, psoriasis can provoke pathologies of the cardiovascular and endocrine systems.
A general urine test is also often prescribed. Disorders related to the excretory system may prevent the prescription of certain medications.
The general urine test includes a physico-chemical examination of the urine (color, density, composition) and a microscopic examination of its sediment. A general urine test is prescribed to check the condition of the body, identify pathologies of the urinary system, gastrointestinal tract, endocrine, infectious and inflammatory diseases.
For the same reason, according to clinical recommendations, tests for HIV and hepatitis are prescribed. Against the background of these infections, the disease can be more severe.
Also, when preparing for treatment, women should take a pregnancy test - for example, take a blood test for beta-hCG. The fact is that many systemic drugs, which are most often prescribed for the treatment of psoriasis and give a good effect, are contraindicated during pregnancy.
The study allows you to diagnose pregnancy in the early stages and identify its complications. In artificial abortion, it is used to evaluate the effectiveness of the procedure. In oncology - for the diagnosis of hormone-producing tumors.
If you complain of joint pain, the doctor will refer the patient for an MRI, CT or X-ray to confirm or rule out psoriatic arthritis. If joint inflammation is confirmed, the dermatologist will recommend an examination by a rheumatologist.
Treatment of psoriasis
If the affected skin area is small, patients are prescribed topical corticosteroid creams or ointments. They suppress inflammation and reduce the manifestations of the disease.
In addition, the doctor can prescribe local analogues of vitamin A or vitamin D. Such drugs relieve inflammation, accelerate the exfoliation of the stratum corneum of the skin and slow down the growth of psoriatic plaques. The use of skin moisturizers from pharmacy dermatocosmetic lines is also recommended.

Mild psoriasis is often treated with topical ointments and creams.
In moderately severe to severe psoriasis, systemic treatment may be required - in the form of classic immunosuppressants and genetically engineered biological drugs in the form of tablets or subcutaneous injections. They have a pronounced effect, but require careful examination before use.
Systemic glucocorticosteroids in psoriasis are contraindicated and can only be prescribed by a doctor in certain (extremely difficult) situations and in hospital settings. Otherwise, such treatment can lead to a significant deterioration of the condition.
Psoriasis is also treated with phototherapy: ultraviolet light of a certain spectrum is directed at the plaques. Many physical therapy offices have special lights for this type of treatment.
The most modern and effective way to treat psoriasis is monoclonal antibodies (genetically engineered biological therapy). These drugs can block some stages of the inflammatory response, for example certain cytokines Cytokines Proteins, which are mainly produced by the immune system's protective cells, provoke inflammation and the growth of plaques in psoriasis.
Prevention of psoriasis
There is no specific prevention that can prevent the development of psoriasis.
In general, it is recommended to lead a healthy lifestyle: give up alcohol and smoking, do sports, eat a healthy and balanced diet.
People whose relatives have psoriasis should be more careful with their skin: moisturize it regularly, avoid hypothermia, prolonged exposure to the sun, and avoid visiting solariums. Tattoos are not recommended if you have a hereditary predisposition to psoriasis.
Forecast
Psoriasis is a chronic pathology, like all autoimmune diseases. It is impossible to completely cure psoriasis.
However, timely and correctly selected treatment can allow the patient to achieve long-term remission - a period of asymptomatic disease.
Frequently asked questions
How is psoriasis transmitted?
Psoriasis is not contagious. It's an autoimmune disease - it occurs when a person's immune system malfunctions and mistakenly attacks skin cells. The disease has a hereditary (genetic) predisposition, meaning it can be inherited.
How does psoriasis manifest itself?
In most cases of psoriasis, large red, scaly plaques appear on the surface of the skin. They can be very itchy and even painful. Most often, psoriatic patches appear on the elbows, knees, torso and scalp.
Which doctor treats psoriasis?
A dermatologist treats psoriasis.
Can people with psoriasis be accepted into the army?
With a mild form of psoriasis, they can be assigned to category B - "limited suitability". A conscript with moderate or severe psoriasis can be considered unfit for military service. In each specific case, the decision is made individually during a medical examination.


















